An epileptic seizure is not a disease in itself but the sign of an abnormal functioning of the brain.
Most eplileptic seizures will occur while a cat is relaxed and resting quietly. Many types of epileptic seizure are described in humans, dogs or cats, although they usually come down to two major categories: partial and generalised.
Generalised seizures
Generalised seizures are usually easy to recognise and are characterised by sudden collapse, loss of awareness, violent shaking of all four limbs, chewing and/or twitching of the face, and often salivation, urination and defecation. These signs last about one to three minutes. Some cats may have one seizure following another one with short recovery in between (cluster seizure) or no recovery at all (status epilepticus). Prior to the actual seizure, the cat may show changes in behaviour such as salivation, growling or pacing. Recovery from a seizure may take a few seconds to a few hours, during which the cat may appear disorientated, blind and wobbly.
Partial seizures
Compared with dogs, cats more commonly exhibit partial seizures. These seizures only affect part of the body and are much more difficult to recognise. They may manifest as drooling, eyelid or facial twitching, excessive vocalisation, growling, and abnormal head, neck or limb movements. They may progress to generalised seizures and they may occur several times throughout the day (cluster seizure). Providing a video recording of the event to your veterinarian is helpful to ascertain if your cat is truly having an epileptic seizure. In a situation when an event is vague and it is unknown whether it is a true seizure, an electroencephalogram (EEG) may be considered to evaluate brain function during the event, although this is not commonly performed even in specialist centres. Although seizures in cats are believed to occur less commonly than in dogs, affected cats tend to experience high seizure frequency whatever the type and underlying cause.
What is epilepsy?
Epilepsy is not a specific disease but a chronic condition characterised by recurrent epileptic seizures. It is caused by an abnormality within the brain itself (see below primary and secondary epilepsy). A cat having a single epileptic seizure does not have epilepsy, as the seizures are not recurrent. If the epileptic seizures occur because of a problem elsewhere in the body, for example a low sugar level in the blood which will starve the brain cells of essential fuel, this is not epilepsy.
What to do while a cat is having a seizure
Although a seizure is a frightening experience for any cat owner, it is important to try to remain calm and not to interfere. Ensure that the cat is not at risk of injuring itself, for example by falling down stairs or off furniture. When the cat starts a seizure, make a note of the time. Most seizures will stop on their own within one to three minutes, although it may take a few minutes to a few hours for the cat to completely recover. If a seizure lasts for a very long period of time (over five minutes for the actual convulsion), or is followed by other seizures close together (cluster seizures), veterinary assistance should be immediately considered.
What is causing the epileptic seizure?
Causes of epileptic seizures can be found inside the brain (intracranial causes) or outside the brain (extracranial causes).
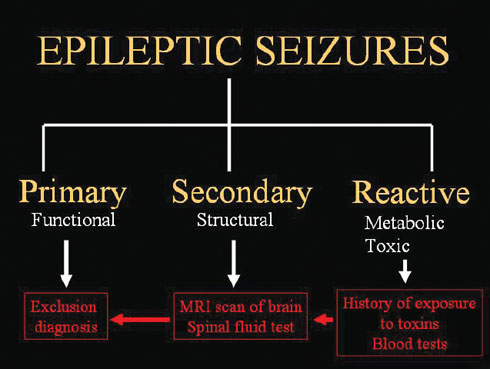
Poisons and metabolic diseases represent extracranial causes. In these cases, the brain is perfectly healthy but reacts by seizuring to a toxin ingested by or applied to the animal, a change in the blood composition caused by a metabolic problem (eg, liver or kidney disease, low calcium or low sugar level), high blood pressure or abnormal heart rhythm. Hence the term ‘reactive epileptic seizures’ is often used to describe this category of causes. With toxic causes, recurrent seizures are not expected unless the cat is exposed again to the toxin.
Intracranial causes are divided into primary and secondary epilepsy. In the case of secondary epilepsy, the epileptic seizures are a sign of a structural disease in the brain. This disease might be a brain tumour, an inflammation or infection of the brain (encephalitis), a brain malformation, a recent or previous stroke or head trauma. Epileptic seizures may occur alone or be associated with other symptoms (circling, blindness, wobbliness, restlessness and/or sleepiness).
In the case of primary epilepsy (also known as idiopathic epilepsy), there is no disease in the brain but the epileptic seizures are caused by a functional problem (chemical imbalance between excitatory and inhibitory messengers of the brain). Cats with primary epilepsy tend to experience their first seizure at a young adult age. While the true incidence of primary epilepsy in cats is unknown, it has been suggested that between 21 and 59% of cats with seizures are primary epileptics. Primary epilepsy in dogs is usually genetic in origin; however, there is little evidence of this in the cat.
Causes and investistigations of epileptic seizures
What tests can be done to investigate the cause of seizures in a cat?
The diagnosis of primary epilepsy is unfortunately a diagnosis of exclusion after elimination of extracranial metabolic and intracranial structural causes. There is no definitive diagnostic test for this condition and all investigations (blood test, MRI scan or CT scan of the brain and CSF analysis — see below) will come back as normal.
Diagnosis of an extracranial cause of epileptic seizures is based on a known exposure to a toxin by the owner and on blood test. The latter is important to eliminate the possibility of kidney, liver and other organ malfunction. Blood pressure evaluation should also be considered in older cats where high blood pressure (often secondary to an overactive thyroid gland, chronic kidney failure and/or heart disease) is a common cause of late-onset seizures.
Diagnosis of secondary epilepsy is based on looking for brain disease using MRI or CT scan of the brain and CSF analysis. MRI stands for magnetic resonance imaging and has become an essential tool in the investigation of neurological disease such as epilepsy. It helps diagnose intracranial causes of seizures such as brain tumours, encephalitis (ie, inflammation or infection of the brain), stroke or malformed brain. Although it is a non-invasive and painless procedure, it requires putting the cat through a general anaesthestic. CT scan stands for computed tomography. It is an X-ray technique where a computer is used to reconstruct cross-sectional images of the animal in the scanner. Compared with MRI, CT gives less detail of soft tissue such as the brain. CSF stands for cerebrospinal fluid which is the fluid that bathes the brain and spinal cord. CSF collection (also referred as a spinal tap) is another essential tool in the investigation of brain disease. This fluid can be collected from either the back of the neck (cisternal puncture) or the lower part of the back (lumbar puncture).
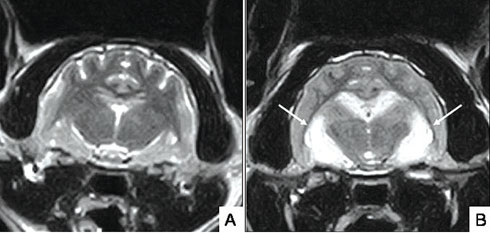
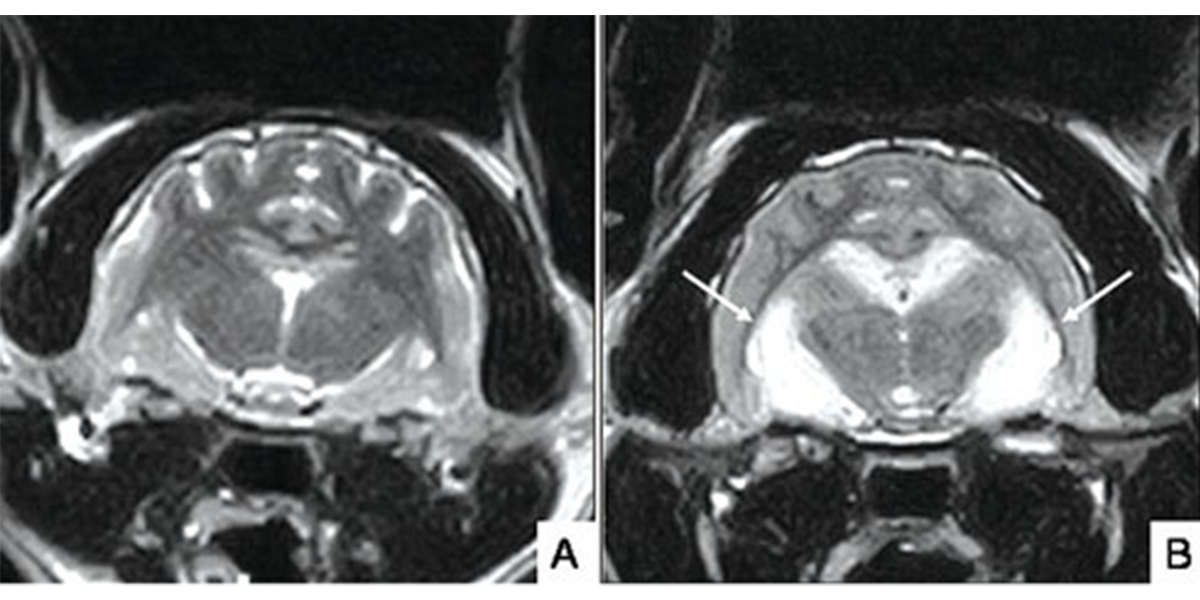
MRI scan of the brain of a normal cat (A) and cat with suspected seizure-induced brain damage (hippocampal necrosis) [white arrows]. Cat (B) presented with acute generalised seizures and behavioural changes including aggression, salivation and disorientation.
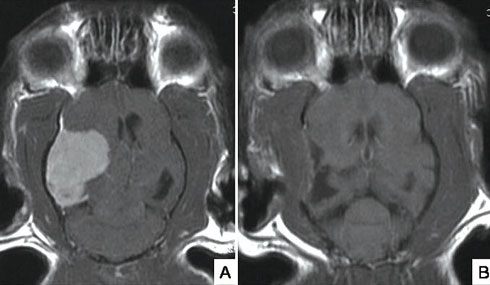
Brain tumours are a potential cause of epileptic seizures, especially in older cats. Scan A shows a large meningioma (benign tumour of the meninges, the lining of the brain) in an 11-year-old cat presented with recent onset of epileptic seizures and circling to the left side. This type of tumour is often amenable to surgical resection with very good outcome in most cats. Repeat MRI scan (B) two months after surgical resection shows complete removal of the tumour.
How are epileptic seizures treated?
Treatment of epileptic seizures should primarily focus on the underlying cause if one can be identified. Treatment of primary epilepsy consists of long-term (often life-long) use of anti-epileptic drugs (see below when to start treatment). Many drugs can be used to this effect in cats including phenobarbital, levetiracetam, zonisamide, gabapentin and pregabalin. The treatment for epileptic seizures does not aim to cure the epilepsy but aims to ‘control’ it. A treatment is usually considered successful if the cat is seizure-free or the frequency of seizures has been reduced by at least 50% and no or minimal side effects of the medication are observed. It is therefore important to keep a seizure log, detailing the number of seizures as well as specific features of the seizures (ie, duration, severity, type of manifestation observed, etc).
When treatment is not effective (ie, the cat does not have a reduction in seizure frequency of 50%, or there is no change, or an increase in seizure frequency), the treatment plan must be re-evaluated with your veterinarian. Causes of failure to respond to antiepileptic treatment include: incorrect diagnosis (causes of epileptic seizures other than epilepsy), inadequate dosage of medication, or the cat becoming ‘resistant’ (or refractory) to the anti-epileptic effect of the drug. Given that primary epilepsy is a condition that cannot be cured, it is very likely that the cat will have to stay on treatment for the rest of its life. Antiepileptic drugs should never be stopped abruptly as ‘withdrawal seizures’ may occur. Dosage reduction should only be considered if the cat remains seizure-free for at least a year; the medication should be tapered off gradually over many months.
When to start anti-epileptic treatment
The decision to start anti-epileptic treatment is still a subject of controversy. Cats with a single seizure or isolated seizures separated by long periods of time do not require treatment. Maintenance anti-epileptic treatment is recommended in any of the following circumstances:
- When a cat is having more than one seizure a month, has more than one cluster event or experiences status epilepticus;
- When seizures occur secondarily to a structural disease of the brain or after a head injury (particularly if seizures begin within the first week of a head injury);
- When the seizures increase in frequency or severity.
Thank you for visiting our website, we hope you have found our information useful.
All our advice is freely accessible to everyone, wherever you are in the world. However, as a charity, we need your support to enable us to keep delivering high quality and up to date information for everyone. Please consider making a contribution, big or small, to keep our content free, accurate and relevant.
Support International Cat Care from as little £3
Thank you.
Donate Now