Just as in humans and dogs, cats have different blood groups. These are important as the blood groups determine the compatibility of blood.
There are three major feline blood groups: A, B and AB. Group A is the most common, but group B is quite common in certain pedigree breeds. Group AB appears to be rare in all breeds.
Because pedigree cats in different countries are sometimes bred from quite different gene pools, in some cases the frequency of blood group A and group B cats can vary between countries so the likely blood group of any individual cat should never be assumed.
Determination of blood groups
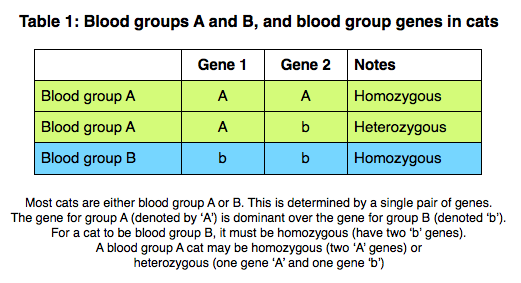
A cat’s blood group is determined genetically. A single pair of genes are generally responsible for determining the blood group and the gene for group A is dominant to the gene for group B.
This means that a cat which is blood group A may have either two type A genes (termed homozygous – two genes the same – for type A), or may have one type A gene and one type B gene (termed heterozygous, having two different genes). In a heterozygous cat, because the A gene is dominant, it will still be blood group A. For a cat to be blood group B, it must carry two type B genes (ie, it is homozygous for type B) – see Table 1. The blood group AB is inherited independently and the AB gene appears to be dominant to the B gene, but recessive to the A gene.
Depending on the parent cats’ genotypes (what genes they carry), a variable proportion of kittens from a mating may be group A or group B. However, if two group B cats are mated together all the kittens will also be type B (as both parents will be homozygous for the ‘b’ gene).
Although blood group A cats are generally the most common, the frequency of type A and B cats varies between countries and between different breeds of cat. For example, the Siamese and some related breeds appear only to have blood group A, while other breeds may have as many as 50% group B cats.
A cat’s blood group can be determined quite simply by tests that are available to use within a veterinary clinic (such as card tests or immunochromatography tests), or in a diagnostic laboratory using similar or more advanced techniques. These tests are usually very reliable. In addition, the genetic make-up of a cat (what blood type genes it is carrying) can be found by sending a blood sample or a cheek swab to a veterinary genetics laboratory.
In an emergency, if tests to determine blood types are not available, compatibility between two cats can also be checked by performing a cross-match.
Blood group incompatibility
Blood group B cats all have naturally occurring high levels of anti-A antibodies in their blood. Antibodies are part of the immune system and this means that if a type B cat were to receive blood from a type A donor, this could cause a severe and even fatal reaction because the immune system would recognise the type A blood as ‘foreign’ and attack it.
Some group A cats also have naturally-occurring anti-B antibodies, meaning that they too may develop severe reactions if given incompatible blood.
Blood transfusions are sometimes needed in cats, and this can be a life-saving procedure in some cats with severe anaemia. If performed properly and with care, blood transfusions are also very safe, but transfusion reactions can be a major problem in cats. Because of their naturally-occurring antibodies, even a first transfusion can be incompatible in cats and cause a major (life-threatening) transfusion reaction.
This means that cats should always be blood typed and/or cross-matched if they need to receive blood and when they donate blood to ensure any transfusion is compatible.
Neonatal isoerythrolysis

Kittens affected by neonatal isoerythrolysis may develop jaundice, causing their skin to appear yellow.
(picture courtesy of Dr Urs Giger)
Any antibodies present in the blood of a queen (female cat) will also be passed into her milk and colostrum (the first milk produced) if they are feeding a litter of kittens. During the first 24 hours of life, a kitten’s intestine is specially adapted to be able to absorb these antibodies so that the kittens can acquire ‘passive protection’ from the queen – ie, the absorbed antibodies will help protect the kitten against diseases in the early weeks of life.
This process is highly beneficial for the kitten, but it can sometimes cause problems with blood groups and blood incompatibilities. If the queen is of blood group B, she will have naturally-occurring anti-A antibodies. If she is mated to a type A tom cat, some of the resulting kittens will be type A and when they feed on the queen’s milk in the first 24 hours of life they will absorb the anti-A antibodies, as well other protective antibodies. The anti-A antibodies will then destroy the kitten’s red blood cells just as if there had been an incompatible blood transfusion. This is a condition known as neonatal isoerythrolysis. This can be a significant cause of death in young kittens in certain breeds (especially those with high numbers of both type A and type B cats).
This disease does not occur in type B kittens born to a type A queen, as type A cats have much lower levels of antibodies against the type B blood cells and often no antibodies at all.
What to look for in affected kittens
The kittens will all be normal at birth but, soon after they have suckled milk, any group A (or AB) kittens in the litter may start to show signs of disease.
The severity of the signs is very variable, probably largely determined by the amount of anti-A antibodies the kitten has absorbed:
- Sudden death, with no prior warning signs in some kittens
- Most affected kittens will appear to ‘fade’ over a few days – they will stop suckling from the queen, become weak, often appear pale and may become jaundiced (yellow)
- Affected kittens usually pass red coloured urine, due to the presence of haemoglobin (released from the breakdown of red blood cells) in the urine
- Mildly affected kittens may show few signs, but the tip of their tail (and sometimes ears) may gradually die off. This is because the antibodies against the red blood cells may prevent normal circulation to the extremities
- Some kittens remain unaffected showing no signs of disease
Treatment of affected kittens
Once the kitten has absorbed the antibodies it is very difficult to treat the problem.
- If recognised in the first few hours of life, the kitten should be removed from the queen for the remainder of the first 24 hours of life to prevent absorption of further anti-A antibodies from the colostrum
- It may be possible to transfuse the kitten with washed red cells from a group B cat (eg, the queen) to supply type B red blood cells which will not be destroyed by the anti-A antibodies. This is often not possible, but when is considered, the cells must be washed first to remove the serum (and anti-A antibodies) to prevent further damage to the kitten’s existing type A red cells. Generally, the problem is recognised too late for this to be helpful, and there are very real, practical difficulties in providing a blood transfusion to a newborn kitten
Preventing neonatal isoerythrolysis
As treatment is rarely possible, it is much more important to prevent this problem from occurring. The situation is most likely to arise in pedigree cats, especially where there is quite a high frequency of both type A and type B cats in the breed. In these situations, the blood type of cats being used for mating should always be determined beforehand. Several approaches can then be taken.
- Avoid using group B cats for breeding altogether. This avoids the problem, but may also limit the pool and choice of breeding cats, which may be undesirable for other reasons.
- Only mate group B queens with group B toms. This will also avoid the problem, but again will limit the choices for matings. All the offspring of such matings will be group B so this approach may have a tendency to gradually increase the proportion of group B cats within a breed.
- Prevent type A kittens from suckling colostrum from a group B queen during the first 24 hours of life. This method has been used by many breeders, and can be successful. It requires blood typing newborn kittens using blood from the umbilical cord. Type A and AB kittens need to be removed from the queen, but any group B kittens in the litter can be left to suckle from the queen. Removed kittens have to be hand-reared for the first 24 hours of life (or placed with a type A foster queen that is producing milk), after which it is safe to put them back with the queen as they will no longer have the ability to absorb antibodies from their intestine.
Approximate frequency of type B cats in various breeds
Note this is for guidance only and will vary between countries and regions
Breeds with only type A or a low frequency of type B (less than 10%)
Breeds with an intermediate frequency of type B cats (10-25%)
Breeds with a high frequency of type B cats (more than 25%)
For more information regarding blood and blood product collection and transfusion, please see:
https://icatcare.org/advice/blood-products-transfusion/
Thank you for visiting our website, we hope you have found our information useful.
All our advice is freely accessible to everyone, wherever you are in the world. However, as a charity, we need your support to enable us to keep delivering high quality and up to date information for everyone. Please consider making a contribution, big or small, to keep our content free, accurate and relevant.
Support International Cat Care from as little £3
Thank you.
Donate Now