The liver is a vital organ, located in the abdomen just behind the diaphragm. The liver has a very wide-ranging role in maintaining normal health and metabolism through functions such as:
- Aiding digestion (especially of fats);
- Synthesis of proteins and hormones;
- Regulating energy and protein metabolism;
- Metabolism and elimination of toxic and waste products;
- Immune regulation.
There is a direct blood supply from the gut to the liver, and partly because of this the liver is vulnerable to toxic injury as any poisons that are eaten will rapidly reach the liver. Cats also have an increased suceptibility because they lack some metabolic pathways in the liver that would be able to deal with some toxins.
The liver can also be affected by a variety of disorders, and other diseases (eg, diabetes mellitus, hyperthyroidism, lymphoma) will also sometimes cause damage to the liver.
The liver has an enormous reserve capacity which means that actual liver failure occurs rarely as more than two-thirds of it has to be severely affected. The liver also regenerates well, which means that recovery is often possible even after severe liver disease.
Signs of liver disease
Signs of liver disease in cats are often very vague, such as:
- Inappetence
- Lethargy
- Weight loss
Depending on the cause and severity, other signs such as a fever, increased thirst or vomiting may also be seen. In some cases liver disease may cause fluid to accumulate in the abdomen (ascites); and with more advanced or severe disease, jaundice (yellowing of the gums and skin) may be seen.
Occasionally with either very severe liver disease or with a ‘shunt’ (where blood from the intestine by-passes the liver due to the presence of an abnormal blood vessel or ‘shunt’) toxins that would normally be dealt with by the liver can reach the brain. This can cause abnormal behaviour, disorientation, excess salivation, and even blindness or seizures to develop.
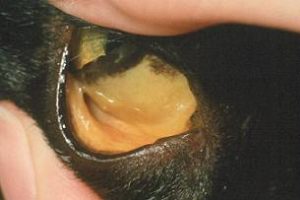
Jaundice can be a sign of liver disease – here the membranes under the eye look yellow
Diagnosis of liver disease
As the clinical signs of liver disease are often vague and non-specific, blood and urine tests are usually needed to identify that liver disease is the underlying cause. Several abnormalities may be seen on blood and urine tests:
- Bilirubin levels may be elevated in the blood and urine
- ‘Liver enzymes’ can be measured in the blood – these are enzymes that are produced in liver cells and if there is damage to the liver (or perhaps obstruction to the flow of bile) these enzyme concentrations in the blood can become elevated. These enzymes may include:
- ALT (alanine aminotransferase)
- ALP (alkaline phosphatase)
- AST (aspartame aminotransferase)
- GGT (gammaglutamyl transferase)
- Bile acids – these are produced by the liver and are important in the digestion of fat in the intestine. In liver disease and where there is obstruction to the flow of bile, bile acid concentrations in the blood may be elevated. While elevated liver enzymes can give information about liver damage, the bile acid test generally gives some information about liver function.
- Haematology – looking at the red and white cells present in the blood – this may give some indications about potential underlying infections or inflammation in the liver.
- Proteins in the blood
Results of blood tests may help confirm the presence of liver disease, but it can be difficult to assess the severity or extent of disease from these tests alone, and they will not reveal the underlying cause. Some of the blood changes can also occur with other diseases as well such as diabetes mellitus and hyperthyroidism, so further tests may also be required to rule these out.
Evaluation of the liver by X-rays (to assess the liver size) and by ultrasound (to evaluate the size and structure of the liver and to look for any evidence of obstruction to flow of bile) can be very helpful in helping to narrow down potential causes of liver disease.
Liver biopsy
Often, to determine the cause of liver disease and the most appropriate treatment, a liver biopsy will be required so that the sample can be looked at by a pathologist (and possibly also sent for culture to rule out bacterial infections). Obtaining a liver biopsy is usually straightforward, but it is important first to make sure that the cat’s blood clots normally (as the liver makes the proteins – or clotting factors – needed for this). A liver biopsy is usually performed under an anaesthetic, and may take the form of a small surgical biopsy, or even a simple needle biopsy.
Common liver diseases in cats
Cats can suffer from a wide range of liver diseases which is why a liver biopsy can be so important in determining the underlying cause and finding the most appropriate treatment. Some important conditions include:
Neutrophilic cholangitis
This is a bacterial infection within the liver causing inflammation. It is usually a result of bacteria migrating up the bile duct and into the liver from the small intestine. It can sometimes be seen with concurrent pancreatic and intestinal disease. Diagnosis requires a liver biopsy as well as culture of the liver biopsy (or a sample of bile from the gall bladder).
Treatment with appropriate antibiotics is required, but the prognosis is usually good if treatment is started promptly.
Lymphocytic cholangitis
This is a non-infectious inflammatory liver disease. The cause is unknown, but may be due to an abnormality with the immune system (immune-mediated disease). Lymphocytic cholangitis often causes enlargement of the liver and may also cause fluid accumulation in the abdomen. Diagnosis is made through examination of a biopsy of the liver.
Treatment consists of anti-inflammatory and immunosuppressive drugs – usually corticosteroids. The prognosis varies depending on the severity, and although it can be good, some cases require prolonged or life-long treatment, and relapses can occur.
Hepatic lipidosis
This is a condition where large amounts of fat accumulates within liver cells – it causes widespread swelling and damage to the liver and can cause severe dysfunction. Hepatic lipidosis is seen most commonly in cats that suddenly stop eating, especially if they were previously overweight. A sudden change in metabolism in these cats (brought on by anorexia) probably causes the fat accumulation. Diagnosis can be confirmed by liver biopsy.
Treatment involves searching for any underlying disease that may have caused or contributed to the hepatic lipidosis. The main treatment of the liver disease itself, is through intensive nutritional support. Cats usually need to be hospitalised and fed special diets via a feeding tube until such time that they are able to feed again for themselves. Although many cats do recover with intensive support, recovery may take months.
Toxic liver damage
Cats are very susceptible to liver damage caused by a wide range of common drugs or toxins that may be quite safe in other species. This is because cats lack some important pathways for metabolising some drugs and toxins that are present in other species. Because of this sensitivity, it is essential that you always consult your vet before giving your cat any medications. See cats and poisons.
Liver tumours
Many different tumours may occur within the liver – some just affecting the liver (primary liver tumours), some that have spread to the liver from elsewhere (secondary liver tumours). Unfortunately many liver tumours carry a poor prognosis, but this is not invariably the case and with some tumours (eg, lymphoma) chemotherapy may be possible. Tumours confined to one lobe of the liver may also be amenable to surgical resection.
Amyloidosis and hepatic peliosis
Amyloidosis is a disease where a type of protein (called amyloid) is deposited within the liver, causing disruption and dysfunction of the liver, and predisposing the cat to liver rupture and bleeding into the abdomen. Some cats are genetically predisposed to this condition.
Hepatic peliosis is an unusual condition where multiple blood-filled spaces develop within the liver. As with amyloidosis, the liver may become very fragile and spontaneous rupture and bleeding into the abdomen can occur.
Other liver diseases
Many other liver diseases can also occur, including portosystemic shunts, toxoplasmosis, feline infectious peritonitis and others.
Treatment of liver disease
Treatment of liver disease depends very much on its cause, which is why additional tests such as a liver biopsy are often needed. In addition to specific treatments, supportive treatment may be helpful in many cases including intravenous fluids where cats are dehydrated, nutritional support, and drugs that may help to support liver function or blood clotting such as:
- Vitamin K
- Ursodeoxycholic acid (UDCA)
- s-adenosylmethionine (SAMe)
- Silybin/Silymarin
Thank you for visiting our website, we hope you have found our information useful.
All our advice is freely accessible to everyone, wherever you are in the world. However, as a charity, we need your support to enable us to keep delivering high quality and up to date information for everyone. Please consider making a contribution, big or small, to keep our content free, accurate and relevant.
Support International Cat Care from as little £3
Thank you.
Donate Now